The acronym DGH A may not immediately reveal its nature to the general public, yet it carries substantial importance in specific domains where administration, policy, governance, and sometimes health or infrastructure intersect. In an age where acronyms proliferate in both bureaucratic and digital spaces, it is important to take a closer look at what DGH A truly stands for, the scope of its activities, and how it contributes to larger structural frameworks that affect people’s daily lives.
This article takes a holistic and detailed approach to understanding DGH A—interpreting it in context, unpacking its operational roles, explaining its relevance to public systems, and offering insights that help demystify its core responsibilities. For students, professionals, policymakers, or the curious citizen, learning about the purpose and inner workings of such an entity equips one to better navigate and participate in systems of governance or sectoral administration where DGH A plays a role.
Let’s begin by examining what DGH A refers to in practical terms, how it might function within governmental or semi-governmental frameworks, and why its operational structure matters in the broader administrative ecosystem.
What Does DGH A Stand For?
To begin, DGH A is an acronym that typically stands for Directorate General of Health – A, with the “A” often indicating a particular division, classification, or regional office. In many national governance frameworks, especially in countries with centralized bureaucratic structures, the term “Directorate General” refers to a high-ranking administrative body responsible for setting standards, formulating policy, implementing national programs, and overseeing compliance within a specific domain.
Thus, when we refer to DGH A, we are typically discussing a department or division under the Ministry or Department of Health, usually tasked with responsibilities such as:
- Healthcare delivery oversight
- Public health infrastructure and planning
- Policy drafting and implementation
- Regulation and quality control in medical services
- Program evaluation and statistics
The “A” suffix might denote Region A, Sector A, or Department A, depending on the country or administrative structure. In some contexts, it could also refer to Division A in a broader Directorate, indicating a specialization in a sub-area like Primary Health Services, Medical Education, or Communicable Diseases.
The Role of Directorate Generals in Government
To understand DGH A more deeply, we must contextualize it within the role of Directorates General (DGs) in government.
A Directorate General is often a technical executive arm of a ministry, where strategic decisions made by ministers and lawmakers are translated into actionable programs, inspections, monitoring systems, and regulatory policies. The DG is responsible for ensuring that national or regional policies are implemented in accordance with budgetary, legal, and operational standards.
Key characteristics of a DG’s function include:
- Operating under a ministerial mandate
- Overseeing subordinate units and regional branches
- Acting as the link between policymakers and frontline service providers
- Designing policy tools, forms, and procedural mechanisms
- Offering expert consultation to ministries and legislators
- Collecting and analyzing data to guide policy adjustments
Therefore, DGH A, as a health-related DG, serves to translate national health strategies into operational reality, managing everything from disease control measures to hospital oversight or regional health audits.
Organizational Structure of DGH A
Most Directorate Generals, including health ones, follow a tiered organizational hierarchy that aligns authority with function. At the top is typically a Director General, who is often a senior civil servant, medical expert, or administrative leader appointed by the government. This individual directs a network of deputy directors, assistant directors, section officers, analysts, and administrative staff.
Within DGH A, you may find the following structural layers:
- Director General: The executive head and strategic decision-maker
- Deputy Directors: Oversight of key thematic areas (e.g., maternal health, emergency medicine)
- Program Coordinators: In charge of specific government programs or mission goals
- Monitoring and Evaluation Officers: Analyze data for program success or shortfalls
- Administrative Cells: HR, finance, procurement, and IT support
- Field Operatives or Inspectors: Oversee implementation at hospitals, clinics, or community centers
DGH A may also coordinate closely with district or provincial health officers, forming a bridge between federal policy and grassroots delivery. This helps ensure uniformity in health outcomes across different regions and demographics.
Core Responsibilities and Mandates of DGH A
The actual responsibilities of DGH A may vary based on national and regional contexts, but they generally fall into several key categories. These responsibilities define how the Directorate interacts with the health ecosystem and its various stakeholders:
1. Policy Development and Implementation
DGH A plays a crucial role in shaping public health policy in line with government priorities. It drafts operational guidelines, standard operating procedures, and manuals for implementing health missions, including vaccination programs, disease eradication plans, and public awareness campaigns.
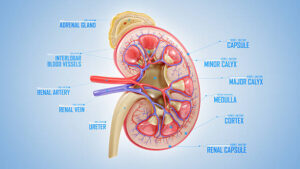
2. Health Infrastructure Oversight
The Directorate is often responsible for planning and maintaining public health infrastructure, including hospitals, clinics, laboratories, and mobile health units. This includes overseeing capital projects, budgeting for equipment, and allocating medical staff.
3. Licensing and Regulation
DGH A may serve as a regulatory authority for licensing hospitals, accrediting medical institutions, and ensuring that health facilities meet safety, hygiene, and clinical standards. It may also set rules for procurement and use of pharmaceuticals or medical technology.
4. Monitoring, Audits, and Evaluation
To ensure transparency and effectiveness, DGH A oversees data collection, performance evaluation, and regular inspections. It measures health indicators, identifies service gaps, and recommends policy tweaks.
5. Emergency and Pandemic Response
In times of health emergencies—such as pandemics, natural disasters, or outbreaks—DGH A becomes a command and coordination center, implementing rapid response teams, managing medical stockpiles, and facilitating inter-agency collaboration.
The Importance of DGH A to Citizens and the Public System
Although DGH A may operate behind the scenes, its influence touches millions of lives. From the quality of care you receive at a government hospital to the vaccination campaign in your neighborhood, its hand is evident. Here’s how its presence supports society:
- Improves access to care through rational planning and funding
- Prevents disease spread via health education and immunization
- Ensures equitable distribution of resources to urban and rural areas
- Monitors unethical practices, fraud, and clinical negligence
- Supports research and innovation in public health solutions
Without a robust entity like DGH A, health governance would suffer from fragmentation, lack of oversight, and inefficiency, especially in countries with large populations and complex administrative layers.
Challenges Faced by DGH A and Similar Directorates
Operating a Directorate General of Health is not without significant challenges. These can include:
- Budget constraints that hinder timely project execution
- Shortage of trained personnel and specialists in remote areas
- Inter-agency coordination hurdles with other ministries like education, sanitation, and environment
- Technological lag in adopting digital health tools
- Bureaucratic delays that slow program implementation
- Public mistrust due to perceived inefficiency or politicization
Addressing these challenges requires reforms, investment, staff training, transparency mechanisms, and the will to modernize processes without compromising public accountability.
DGH A in the Digital Age
With digital transformation accelerating in the healthcare sector, DGH A and its counterparts are moving toward paperless systems, mobile health data collection, and online reporting dashboards. These tools enable quicker decision-making and better outreach.
For instance, DGH A may:
- Develop mobile apps for patient tracking and reporting
- Use GIS mapping to track health facility locations and service gaps
- Launch telemedicine platforms for underserved areas
- Integrate electronic health records to support continuity of care
These steps not only modernize the institution but also empower citizens with access to services and information at their fingertips.
The Future Outlook of DGH A
Looking ahead, DGH A is expected to:
- Play a central role in achieving universal health coverage goals
- Drive climate-sensitive health policies as weather events become more disruptive
- Integrate AI and machine learning to predict and prevent outbreaks
- Collaborate with private healthcare providers through public-private partnerships
- Continue strengthening community-based care models, especially for aging populations
Success will depend on visionary leadership, adequate funding, and a people-centered approach that values both technology and empathy in public health delivery.
Conclusion
In the ever-complex world of public administration, DGH A stands as a pillar of health governance—organizing policy into practice, managing infrastructures that deliver critical services, and ensuring that the health of citizens remains a top priority. Whether through quiet regulation or visible action, its mandate touches every layer of society, from urban centers to rural outposts.
By understanding what DGH A is, how it functions, and why it matters, we empower ourselves not just as informed individuals, but as active stakeholders in the collective well-being of our communities. Clarity about such institutions also enhances civic engagement, enabling us to ask the right questions, demand accountability, and contribute meaningfully to policy discussions in the public interest.
FAQs
1. What is DGH A in the context of government health systems?
DGH A typically refers to a specific division or region of a Directorate General of Health, responsible for executing public health policies and infrastructure oversight.
2. Is DGH A a national or regional body?
It can be either, depending on the administrative setup. The “A” may denote a regional office, division, or specialization within the broader health directorate.
3. What does DGH A do for the public?
DGH A helps implement health programs, regulate healthcare facilities, respond to emergencies, and ensure equitable access to health services.
4. Who leads DGH A and how are they appointed?
DGH A is typically headed by a Director General, who is a senior government official or expert appointed by the health ministry or executive branch.
5. Can the public interact with or access services through DGH A?
While it is not a frontline service agency, DGH A indirectly affects services received at clinics and hospitals. Citizens may also engage through public health campaigns, feedback systems, and grievance redressal platforms.
For more information, click here.