In the world of rare diseases, most stories never reach headlines. They unfold quietly, in homes and hospitals, marked by years of misdiagnosis, medical uncertainty, and systemic silence. One such story—deeply personal yet profoundly universal—is that of Amanda Bennitt Wallace, a woman whose life became inextricably linked to Tuberous Sclerosis Complex (TSC). Her journey not only illuminates the challenges of living with a lifelong neurological disorder but also raises larger questions about public health, advocacy, and the importance of research funding.
Amanda Bennitt Wallace did not set out to become a public figure. Yet through her quiet perseverance, informed activism, and community leadership, she has become a central name in the TSC narrative, especially among families seeking both medical clarity and emotional solidarity. For anyone researching TSC Amanda Bennitt Wallace, this article offers an expansive, compassionate, and updated understanding of who she is, the medical condition she lives with, and the broader implications for rare disease support systems.
Understanding TSC: A Primer for Context
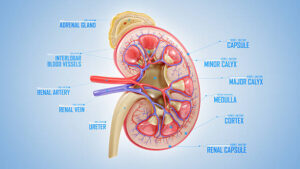
Before diving into Amanda’s story, it’s essential to understand the condition that defines so much of her life. Tuberous Sclerosis Complex (TSC) is a rare, multisystem genetic disorder that causes benign tumors to grow in the brain and other vital organs such as the kidneys, heart, eyes, lungs, and skin. The disease is caused by mutations in either the TSC1 or TSC2 gene, which regulate cell growth. When these genes fail, tumors form.
While TSC is considered rare, affecting about 1 in 6,000 live births, it is one of the most common genetic causes of epilepsy and autism. The symptoms range significantly, from mild skin abnormalities to severe developmental delays and intractable seizures. This wide spectrum makes TSC uniquely difficult to diagnose and manage—often requiring input from neurologists, nephrologists, dermatologists, cardiologists, and psychiatrists.
There is no known cure for TSC, but treatments such as mTOR inhibitors (like everolimus), seizure medications, surgical interventions, and supportive therapies can significantly improve quality of life.
Amanda Bennitt Wallace: A Personal Story of a Complex Diagnosis
Amanda Bennitt Wallace’s connection to TSC is both lived and deeply reflective. She was diagnosed as a child, in an era when public awareness of the condition was virtually nonexistent and the internet had not yet become a hub for patient education. For years, Amanda Bennitt Wallace’s symptoms were misunderstood—frequent seizures, unusual skin growths, and cognitive variances were often dismissed as isolated issues rather than part of a larger syndrome.
Amanda’s parents, like many others in the TSC community, were told to wait and see. It wasn’t until further genetic testing and neurological evaluations in her teenage years that a formal diagnosis of Tuberous Sclerosis Complex was made. By then, Amanda had already endured numerous hospital visits, learning interruptions, and medication side effects—all without a unifying diagnosis.
Her journey from that moment forward became one of transformation—from patient to advocate, from isolated child to community organizer, and from silence to storyteller.
Advocacy Begins at Home: Building a Voice for Others
What separates Amanda Bennitt Wallace from many patients is her decision to publicly embrace her diagnosis not as a limitation, but as a lens through which to understand and impact others. She began by blogging anonymously, sharing snippets of life with seizures, brain scans, social stigma, and medication routines. Her authenticity resonated with other TSC families, who often felt marginalized or misunderstood in conventional medical settings.
As her following grew, Amanda stepped into public roles:
- Speaking at medical conferences about the patient experience
- Advising research committees on ethical study design
- Launching digital support groups for newly diagnosed families
Her voice began shaping the narrative of TSC as not just a clinical anomaly, but a human condition—with fears, humor, setbacks, and hopes.
The Importance of Digital Storytelling
In an era dominated by fragmented attention, Amanda Bennitt Wallace’s long-form storytelling stood out. She rejected superficiality in favor of nuanced, emotionally intelligent commentary on topics like:
- Losing friends due to visible skin lesions
- Navigating college accommodations with a neurological disorder
- Dating while disclosing a chronic genetic condition
- Advocating for inclusive clinical trial participation
One notable viral post described Amanda Bennitt Wallace’s experience during a particularly violent seizure on public transportation, where bystanders filmed instead of helping. It sparked widespread discussion on disability empathy, public awareness, and ethical boundaries in the age of smartphones.
Through platforms like Vimeo, Instagram Live, and patient webinars, Amanda Bennitt Wallace continues to use her story as a platform for visibility, education, and systemic accountability.
Medical Partnerships: From Subject to Stakeholder
Amanda’s growing visibility brought her into contact with medical institutions and advocacy organizations—including partnerships with the Tuberous Sclerosis Alliance and university-based epilepsy research centers. These collaborations shifted Amanda’s role from patient subject to stakeholder and strategist.
Key contributions include:
- Participating in advisory boards shaping clinical trial recruitment language to make it more inclusive
- Helping hospitals design more trauma-informed intake protocols
- Co-authoring papers on neurodiversity and healthcare equity
These contributions are not symbolic; they reflect a new model of research partnership, one where lived experience is considered essential data.
The Gendered Dimensions of TSC
A significant but often overlooked aspect of Amanda’s advocacy is her attention to how TSC presents differently in female-identifying patients. Issues such as hormonal influences on seizure activity, menstruation-related flares, and pregnancy planning often lack rigorous study.
Amanda has spoken openly about:
- Hormonal contraceptives and their interactions with anti-epileptic drugs
- Concerns around hereditary transmission and reproductive planning
- Gender bias in clinical settings when symptoms are dismissed as “anxiety” or “emotional”
By naming the gender gap, Amanda encourages both researchers and patients to push for equity in diagnostics, treatment, and data collection.
Living with TSC in 2025: A Realistic Yet Hopeful Picture
Thanks to evolving treatment protocols and patient advocacy, the landscape for people with TSC in 2025 is improving—but unevenly.
Advances:
- mTOR inhibitors have improved outcomes in kidney and brain tumors
- Early genetic screening is becoming more available
- Digital health tracking enables proactive management of symptoms
Ongoing Challenges:
- Access to care is still limited by geography and insurance coverage
- Neuropsychiatric issues such as aggression, anxiety, and autism-related symptoms remain hard to treat
- Adult patients often fall through care gaps, especially during transition from pediatric providers
Amanda Bennitt Wallace continues to navigate these complexities herself while supporting others. She sees her mission not as “overcoming” TSC but living within its reality with autonomy, humor, and hope.
The Broader Impact: From Personal Story to Public Policy
Amanda’s influence now stretches into policy circles, where she has testified before health subcommittees and written op-eds on:
- Expanding funding for rare disease registries
- Creating national health data portals for conditions like TSC
- The emotional toll of medical debt among rare disease patients
Her work has inspired legislative proposals aimed at improving early intervention funding, insurance flexibility, and patient education mandates—especially in states like Texas and Oklahoma, where TSC diagnoses are disproportionately late due to healthcare access disparities.
Conclusion
The name Amanda Bennitt Wallace may not appear in textbooks or television interviews—yet—but in the landscape of rare disease advocacy, she represents a quiet revolution. Through lived experience, medical collaboration, and digital storytelling, she has reframed TSC not as an ending, but as a platform for empathy, reform, and connection.
Her story is not just about surviving a genetic disorder—it’s about redefining it, and in doing so, offering a new blueprint for what advocacy in the 21st century can look like: intimate, informed, and indefatigably human.
For families grappling with a new diagnosis, for researchers questioning their methodology, or for educators seeking to better understand neurodiversity, Amanda’s voice is a reminder: the person must always come before the pathology.
Frequently Asked Questions (FAQs)
1. Who is Amanda Bennitt Wallace?
Amanda Bennitt Wallace is a TSC patient and advocate known for her work in public storytelling, medical advisory roles, and digital community support around Tuberous Sclerosis Complex.
2. What is Tuberous Sclerosis Complex (TSC)?
TSC is a rare genetic disorder that causes noncancerous tumors to grow in vital organs, especially the brain and kidneys. It often includes neurological and developmental symptoms like epilepsy and autism.
3. How has Amanda contributed to TSC research or advocacy?
Amanda has spoken at conferences, served on advisory boards, written advocacy essays, and consulted on clinical trials, particularly those focused on lived experience and equitable access.
4. Does Amanda Bennitt Wallace use video platforms like Vimeo?
Yes, Amanda has utilized Vimeo and other platforms to share her experiences, including storytelling videos, public education resources, and recorded panels with other patients and doctors.
5. Why is her story significant?
Amanda’s narrative humanizes a complex disorder and has reshaped how patients, researchers, and policymakers approach TSC. She demonstrates how individual voices can drive structural change in healthcare.
For more information, click here.